Allergy Season Oral Health Risk Calculator
Enter your symptoms and habits, then click "Calculate Your Risk Level"
When pollen spikes and your nose starts to itch, the last thing on your mind is your smile. Yet the connection between seasonal allergies oral health is real, and ignoring it can turn a runny nose into gum pain or tooth sensitivity. This guide walks you through what’s happening in your mouth when allergies flare, how to protect your teeth and gums, and when a dentist’s help becomes crucial.
Quick Takeaways
- Allergy‑related mouth dryness lowers saliva, raising decay risk.
- Sinus congestion can cause post‑nasal drip, irritating gums and teeth.
- Antihistamines may worsen dry mouth; choose sugar‑free gum or lozenges.
- Good oral hygiene and rinses help flush allergens and keep plaque down.
- See a dentist if you notice persistent gum swelling, bleeding, or sudden tooth sensitivity during allergy season.
What Are Seasonal Allergies?
Seasonal allergies are an immune response to airborne allergens like pollen, mold spores, or dust mites that appear at certain times of the year. When the body spots these particles, it releases histamine, leading to sneezing, itching, watery eyes, and congestion. In South Africa, spring (September‑November) brings a surge of pollen from grasses and trees, making allergies especially common in regions such as Durban.
How Allergies Affect Your Mouth
Even though allergies primarily target the respiratory system, the mouth is a secondary battlefield. Here are the main ways they interfere with oral health:
- Dry Mouth (Xerostomia): Histamine and many antihistamine medications reduce saliva production. Saliva is the mouth’s natural cleanser; without enough of it, food particles linger, and harmful bacteria thrive.
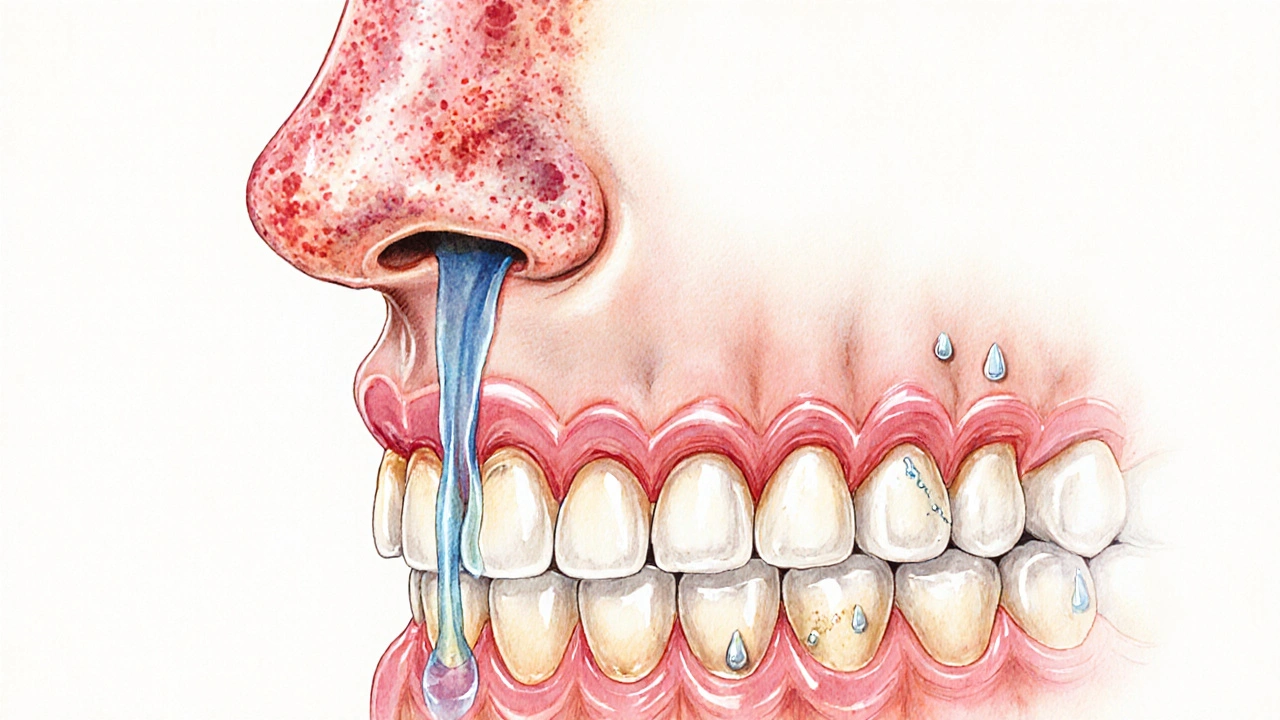
- Post‑nasal Drip: Congested sinuses push mucus down the throat, which can coat teeth and gums with acidic secretions, eroding enamel over time.
- Inflamed Gums: Allergic inflammation can extend to the gingiva, causing redness, swelling, and a higher chance of bleeding during brushing.
- Oral Itchiness and Soreness: Direct contact with pollen particles can irritate the soft tissues of the mouth, making them more vulnerable to ulcerations.
- Altered Taste and Smell: A blocked nose changes how you perceive flavors, sometimes leading to cravings for sugary foods that further feed plaque.
Key Oral‑Health Players in Allergy Season
Understanding the main entities involved helps you target the right remedies.
- Saliva: the fluid that buffers acids, washes away microbes, and supplies minerals for enamel.
- Plaque: sticky biofilm of bacteria that thrives in low‑saliva environments.
- Gingival tissue: gums that can become inflamed from both allergic cytokines and bacterial irritation.
- Enamel: the hard outer layer of teeth that can be softened by acidic post‑nasal drip.
- Antihistamines: drugs that block histamine but often dry out the mouth.
- Mouthwash: a rinsing aid that can help reduce bacterial load and rinse away allergens.
- Dentist: the professional who can spot early signs of allergy‑related oral issues.
Practical Steps to Protect Your Teeth and Gums
Turn the allergy season into a chance to boost your dental routine. Follow these evidence‑backed actions:
- Stay Hydrated: Sip water throughout the day. Aim for at least 2liters, and keep a bottle handy during outdoor activities where pollen counts are high.
- Chew Sugar‑Free Gum: Stimulates saliva flow without adding sugar. Xylitol‑based gums have the added benefit of lowering plaque bacteria.
- Choose a Gentle, Fluoride‑Rich Toothpaste: Fluoride supports enamel repair, especially important when post‑nasal drip creates acidic conditions.
- Use an Alcohol‑Free, Antimicrobial Mouthwash: Look for ingredients like cetylpyridinium chloride or chlorhexidine (low‑concentration) to clean the mouth without drying it out further.
- Rinse After Allergy Medication: If you take antihistamines or nasal sprays, swish with water or a mild mouthwash afterward to flush residual chemicals.
- Maintain a Two‑Minute Brushing Routine: Brush twice daily, focusing on the gum line where plaque can accumulate quickly when saliva is scarce.
- Floss Daily: Use floss or interdental brushes to remove food particles that saliva can’t reach.
- Consider a Saliva Substitute: Over‑the‑counter saliva lozenges or sprays can provide temporary relief on particularly dry days.
When to Seek Professional Dental Care
Most allergy‑related mouth changes improve once the season passes, but some signs demand a dentist’s attention:
- Gums that bleed consistently, even with gentle brushing.
- Persistent bad breath that doesn’t improve with oral hygiene.
- Sudden tooth sensitivity to hot or cold foods, especially if it lasts longer than a few weeks.
- Visible sores or ulcerations that don’t heal within ten days.
- Noticeable shifts in bite or jaw comfort, possibly linked to sinus pressure.
During an appointment, the dentist may check for enamel erosion, take X‑rays if decay is suspected, and offer professional fluoride treatments or a custom mouthguard if you grind teeth due to allergy‑induced stress.

Nutrition Tips to Counteract Allergy‑Driven Oral Issues
What you eat can either soothe or aggravate allergy‑related oral problems.
- VitaminC‑Rich Foods: Oranges, strawberries, and bell peppers boost gum health and support the immune system.
- Omega‑3 Fatty Acids: Found in salmon, walnuts, and flaxseeds, they help dampen inflammatory responses.
- Calcium‑Rich Dairy: Milk, cheese, and yogurt provide the minerals needed for enamel repair.
- Avoid Acidic Snacks: Citrus juices, soda, and sports drinks increase enamel wear, especially when saliva is low.
- Limit Sugary Treats: Bacteria love sugar; highglycemic snacks fuel plaque formation.
Managing Allergies Without Sacrificing Oral Health
Balancing effective allergy relief with mouth‑friendly habits is doable. Here are some strategies:
- Opt for Non‑Sedating Antihistamines: Many newer antihistamines (e.g., loratadine, cetirizine) cause less dryness than older ones like diphenhydramine.
- Use Nasal Sprays with Saline: Saline rinses keep nasal passages clear without drying the mouth.
- Try Immunotherapy: Allergy shots or sublingual tablets gradually desensitize you to pollen, reducing the need for daily meds.
- Schedule Dental Check‑Ups Early in the Season: A professional cleaning before pollen peaks gives your mouth a clean slate.
- Keep a Symptom Diary: Note when gum swelling or tooth sensitivity spikes; cross‑reference with pollen counts to spot patterns.
Comparison: Common Allergy Symptoms vs. Oral‑Health Effects
| Allergy Symptom | Oral‑Health Effect | Typical Mitigation |
|---|---|---|
| Runny nose & post‑nasal drip | Acidic coating on teeth → enamel softening | Rinse with water or mild mouthwash after episodes |
| Congestion | Reduced airflow → mouth breathing → dry mouth | Use humidifier; stay hydrated; chew sugar‑free gum |
| Itchy eyes & sneezing | Frequent rubbing introduces bacteria to eyelids and cheeks → potential gum irritation | Wash hands regularly; avoid touching face |
| Medication (antihistamines) | Decreased saliva production → higher plaque risk | Saliva substitutes; Xylitol gum; fluoride mouthwash |
| Sinus pressure | Jaw discomfort; possible temporomandibular strain | Warm compress; gentle jaw stretches; dental check‑up if persistent |
Frequently Asked Questions
Can seasonal allergies cause cavities?
Yes, indirectly. Antihistamines and nasal congestion often dry out the mouth, lowering saliva’s protective effect. Without enough saliva, plaque builds faster, increasing the risk of cavities.
Why does my gum bleed more during pollen season?
Allergic inflammation releases cytokines that can make the gingival tissue more fragile. Combined with reduced saliva, plaque irritates the gums, leading to bleeding during brushing.
Are there allergy medicines that don’t dry my mouth?
Second‑generation antihistamines such as loratadine, cetirizine, and fexofenadine are designed to be less sedating and typically cause less dryness than first‑generation options like diphenhydramine.
Should I see a dentist if my teeth feel extra sensitive during allergy season?
If sensitivity lasts more than a couple of weeks or interferes with eating, book an appointment. A dentist can check for enamel erosion, recommend desensitizing toothpaste, or apply a fluoride varnish.
Can I use a regular mouthwash while taking antihistamines?
Choose an alcohol‑free mouthwash. Alcohol can worsen dryness, while an antimicrobial rinse with cetylpyridinium chloride or low‑dose chlorhexidine helps control plaque without further drying the mouth.


Tammie Foote
October 5, 2025 AT 13:24We all have a responsibility to keep our bodies in fighting shape, especially when nature throws pollen at us like confetti. Ignoring the link between allergies and oral health is basically saying we don't care about our own well‑being. The extra dry mouth that antihistamines cause is a perfect breeding ground for decay, and that's something we can’t just shrug off. So brush twice, floss, and stay hydrated – it's the least we can do for ourselves.
Jason Ring
October 5, 2025 AT 16:11i totally get the point about staying hydrated, but i also think people get overwhelmed by all the tips. it's easy to just grab a water bottle and go, but sometimes we forget to actually sip throughout the day. also, a quick rinse after using antihistamines helps a lot. just a gentle reminder, no need to stress.
Kelly Hale
October 5, 2025 AT 18:57When the pollen clouds roll in, it's not just a simple sneeze‑fest; it's a full‑blown battlefield for our mouths, and the stakes are higher than most people realize. First, the histamine surge dries out the saliva, turning our mouths into desert plains where bacteria throw a party. Then the post‑nasal drip drips acid onto enamel, eroding it like tiny, relentless sandstorms. Add to that the fact that many over‑the‑counter antihistamines act like miniature desert suns, scorching the lining of the mouth and making gums fragile. This combination means plaque can set up camp far earlier than in a typical year, and the risk of cavities skyrockets. Moreover, the inflammation from allergic reactions doesn't stay confined to the sinuses; it spreads to gingival tissue, making gums bleed at the slightest brush. Imagine trying to brush your teeth and feeling a fresh stream of blood – that's the narrative many allergy sufferers end up living through. The good news is that we can arm ourselves with a multi‑pronged defense: chew xylitol‑sweetened gum to jump‑start saliva flow, keep a bottle of water within arm’s reach, and rinse with an alcohol‑free antimicrobial mouthwash after each dose of medication. A fluoride‑rich toothpaste will also help remineralize any enamel that has started to soften under the acidic assault. Finally, schedule a dental cleaning before the pollen count spikes; a professional wipe‑down can remove the buildup before it becomes a permanent problem. In short, treat your mouth like a warzone during allergy season – prep, protect, and patrol, and you’ll emerge victorious with a smile intact.
Neviah Abrahams
October 6, 2025 AT 00:31Allergies make your mouth feel like a desert and then you add meds that dry it out you forget that saliva is the first line of defense against decay it’s like turning off the cleaning crew and letting the grime pile up first the gums get irritated and start bleeding even simple brushing can become painful so think about a water rinse after each spray and keep a sugar free gum handy it’s simple but it works
Uju Okonkwo
October 6, 2025 AT 03:17Hey everyone, just wanted to add that a supportive routine can make a huge difference. If you notice your mouth getting dry, try sipping warm water instead of cold – it feels soothing and encourages saliva production. Also, consider a small bottle of saliva substitute if your symptoms spike. Gentle flossing with a water flosser can be kinder on irritated gums while still removing plaque. Remember, you’re not alone in this – a little extra care now can prevent bigger problems later.
allen doroteo
October 6, 2025 AT 08:51Honestly, all this hype about special mouthwashes is overblown. Plain water does the job just fine, and chewing gum is just a marketing gimmick. If you’re already taking antihistamines, you’re set for dry mouth – there’s nothing you can really do about it.
Corey Jost
October 6, 2025 AT 11:37While I see where the previous comment is coming from, I think it’s worth digging deeper into the whole “plain water is enough” narrative. First of all, water alone doesn’t replenish the minerals that saliva provides, which are essential for enamel remineralization. Second, the act of chewing sugar‑free gum, especially those containing xylitol, actively stimulates salivary flow, which does more than just moisten – it introduces natural buffering agents that neutralize the acids from post‑nasal drip. Moreover, many over‑the‑counter antihistamines have a pronounced anticholinergic effect that inhibits not just volume but also the composition of saliva, reducing its protective enzymes. Therefore, supplementing with a specialized, alcohol‑free antimicrobial rinse that contains cetylpyridinium chloride can provide an extra layer of defense against bacterial overgrowth. Finally, a brief, consistent routine of rinsing after each medication dose creates a habit loop that ensures you don’t forget the extra step during a busy day. So while plain water is a good baseline, adding these targeted measures creates a more robust defense against the cumulative damage that allergy season can inflict on oral health.
Nick Ward
October 6, 2025 AT 17:11Great points everyone! 😊 Just a quick reminder: staying consistent with a two‑minute brush and a gentle floss is the real hero here. If you can, set a timer on your phone – it helps keep the routine solid. Also, an alcohol‑free mouthwash can freshen breath without adding to dryness. Keep smiling! 👍
felix rochas
October 6, 2025 AT 19:57Listen, the pharmaceutical companies don’t want you to know that the “new generation” antihistamines are just a way to keep you buying more meds!!! They intentionally design them to cause dry mouth so you’ll need expensive saliva substitutes and special rinses that they also market. It’s a classic profit‑driven scheme, and we’re all paying the price while they sit on their thrones!!!
inder kahlon
October 7, 2025 AT 01:31Practical tip: keep a small bottle of fluoride rinse at your desk. A quick swish after a dose of antihistamine restores some mineral balance to the teeth and reduces enamel softening.
Dheeraj Mehta
October 7, 2025 AT 04:17Stay positive! 🌟 A little extra water and a minty, alcohol‑free mouthwash can keep that fresh feeling even when pollen is high. Keep up the good work!
Oliver Behr
October 7, 2025 AT 09:51From a UK perspective, we also see more gum irritation in spring, so swapping to a non‑alcoholic rinse is a simple fix.
Tiffany W
October 7, 2025 AT 12:37One must underscore the pathophysiological nexus between histamine‑mediated xerostomia and the demineralization cascade, leveraging fluoride‑augmented remineralization protocols to mitigate iatrogenic enamel compromise.
Rajeshwar N.
October 7, 2025 AT 18:11The data suggests that while antihistamines dry the mouth, the impact varies per individual metabolic profiles. Therefore, a blanket recommendation isn’t adequate; patients should assess their own salivary flow and adjust hygiene practices accordingly.
Louis Antonio
October 7, 2025 AT 20:57Honestly, most of this is just hype. You brush, you floss, you’re fine. No need to overthink it.
Kyle Salisbury
October 8, 2025 AT 02:31I’ve found that a simple water rinse works well for me during pollen spikes.
Angie Robinson
October 8, 2025 AT 05:17It’s obvious that people who ignore the connection between seasonal allergies and oral health are just lazy. The scientific community has spelled out the risks, yet many still brush half‑heartedly and expect miracles. If you’re not willing to take basic preventive steps, you deserve the consequences of gum disease and cavities.
Emmons Kimery
October 8, 2025 AT 08:04Hydrate, rinse, smile 😊